The Effect of Conditioning on OCD - OCD Therapy
Learn more about OCD Therapy in NJ.
In this Blog, You'll Learn
✅ What OCD is and how obsessions differ from compulsions
✅ Myths vs. facts about OCD
✅ How classical conditioning creates fears
✅ How operant conditioning reinforces compulsions
✅ Why conditioning matters for OCD treatment
✅ Coping strategies for managing OCD
✅ Therapy approaches for OCD (CBT, ACT, DBT, EFT, Mindfulness & more)
✅ FAQs, including the role of medication
There is more to OCD than just being “afraid of germs” and wanting to “clean” and be “neat.” Obsessive-Compulsive Disorder (OCD) is when an individual struggles with an obsession(s) or compulsion(s) that cause major distress and anxiety while interfering with their daily routine.
This blog will explore how classical and operant conditioning help explain why compulsions are so persistent and hard to break. This is different from an individual who simply has a “cleaning personality complex.”
Obsessions and Compulsions: What They Are and How They Work
Obsessions
Obsessions are persistent, unwanted, and recurrent thoughts or images. They cause severe distressful emotions like anxiety, fear, and disgust for an individual. Some people with OCD realize how unreasonable these obsessions are but still struggle to ignore them.
Examples of obsessions include:
- Fear of contamination
- Fear of losing a valuable object or forgetting important information
- Fear of things being out of order or unsymmetrical
Compulsions
Complutions, on the other hand, are behaviors or mental acts that become ritualistic for an individual, as they are driven to perform them in response to their obsessions. These behaviors and/or mental acts are performed to reduce the anxiety and other distressful emotions caused by obsessive thoughts. But that doesn’t make these compulsions a healthy coping mechanism.
Examples of compulsions include:
- Cleaning
- Checking
- Counting
- Avoidance
- Mental rituals
👉 As stated, compulsions are performed to reduce anxiety caused by obsessions.
Myths vs. Facts About OCD
Myth: OCD is just about being “clean” or “organized.”
Fact: OCD is a cycle of intrusive thoughts (obsessions) and compulsions, often linked to fear conditioning.
Myth: People with OCD can just “stop” their behaviors if they really want to.
Fact: Compulsions are reinforced through conditioning and are very difficult to break without therapy.
Myth: OCD is rare.
Fact: Millions of people experience OCD, across all ages and backgrounds.
Classical Conditioning in OCD
Classical conditioning is a learning process in which a neutral stimulus becomes associated with a natural response due to being paired with an unconditioned stimulus. After repeated exposure, the neutral stimulus elicits the automatic response on its own.
In OCD, this learning process is referred to as fear conditioning:
- A neutral trigger (like a place or an object) becomes associated with anxiety and fear.
- The unconditioned stimulus (US) gets paired with the neutral trigger (conditioned stimulus), producing the conditioned response.
Example:
- Unconditioned Stimulus (US): Germs
- Unconditioned Response (UR): Anxiety/Fear
- Neutral Stimulus → Conditioned Stimulus (CS): Doorknob
- Conditioned Response (CR): Anxiety from touching the doorknob, even if clean
👉 In this example, classical conditioning explains how a neutral object (doorknob) becomes tied to fear (germs), creating a conditioned response.
Operant Conditioning in OCD
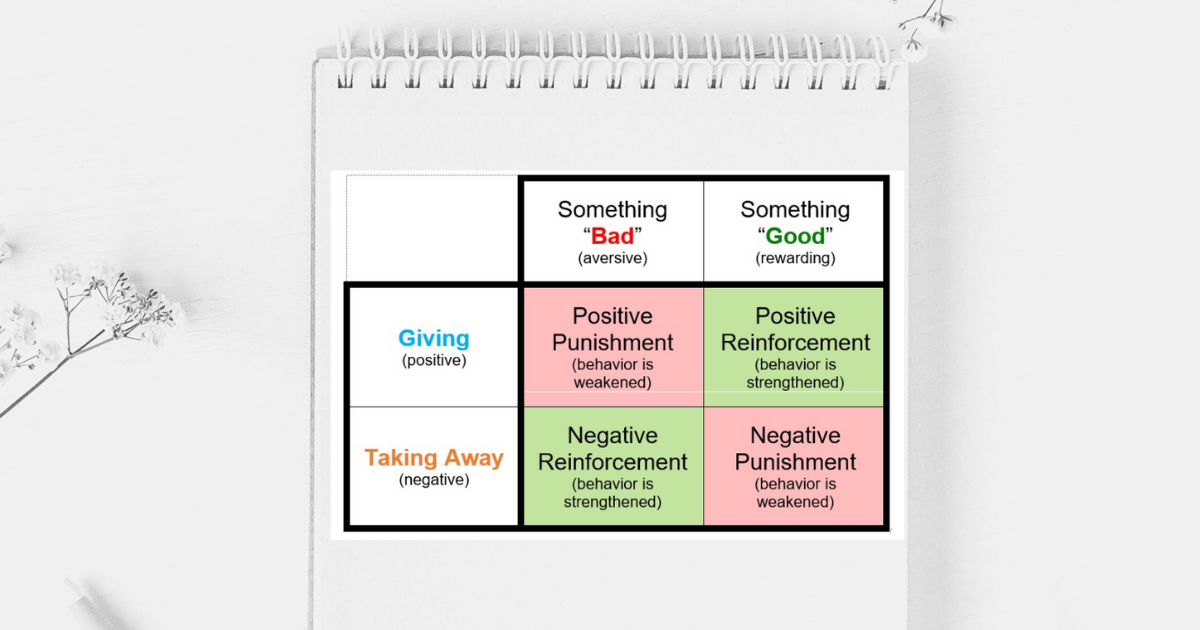
Operant conditioning, like classical conditioning, is also a learning process — but with the addition of punishments and reinforcers. These consequences help either strengthen or weaken a behavior.
In OCD:
- Compulsions are negatively reinforced.
- Performing a compulsion reduces anxiety, creating a sense of relief.
- That relief reinforces the behavior, making it more likely to be repeated the next time anxiety arises.
👉 This cycle explains why compulsions are so difficult to stop.
Why This Matters for Treatment
Understanding how classical and operant conditioning work in influencing OCD symptoms helps explain why exposure therapy is so effective.
- Classical conditioning ties a neutral trigger (like a doorknob) with anxiety (e.g., germs).
- Operant conditioning reinforces compulsions, since they provide short-term relief.
Exposure Therapy for OCD in NJ
One of the main goals of Exposure Therapy is to break the conditioning cycle.
- The individual is exposed to their fear without being able to follow through with their compulsion.
- Over time, repeated exposure reduces the fear and weakens the compulsions.
Coping Strategies for OCD
While therapy is essential, individuals can also try supportive strategies:
- Awareness: Notice when you are engaging in compulsions and how they are reinforcing your anxiety.
- Mindfulness: Practice tolerating distress without immediately turning to compulsions.
- Gradual exposure: Slowly face feared triggers in small steps without completing the compulsion.
How Therapy Helps Break the Conditioning Cycle
Therapists use evidence-based approaches to help break the OCD cycle:
- ACT – Acceptance Commitment Therapy for OCD: Helps clients accept difficult thoughts without acting on compulsions and align actions with personal values.
- Attachment-Based Therapy for OCD: Builds security in relationships and addresses attachment wounds that may intensify OCD fears.
- CBT – Cognitive Behavioral Therapy for OCD: Identifies unhelpful thought patterns and changes compulsive behaviors.
- DBT – Dialectical Behavioral Therapy for OCD: Teaches distress tolerance, mindfulness, and emotion regulation to manage OCD triggers.
- EFT – Emotionally Focused Therapy for OCD: Strengthens emotional awareness and connection in relationships, which can reduce isolation linked to OCD.
- Mindfulness-Based Therapy for OCD: Encourages non-judgmental awareness of thoughts, helping individuals resist compulsive urges.
- Narrative Therapy for OCD: Helps clients reframe OCD as something separate from themselves, reducing shame and self-blame.
- Psychodynamic Therapy for OCD: Explores underlying unconscious conflicts and early experiences that may drive OCD symptoms.
- SFT – Solution Focused Therapy for OCD: Focuses on small, achievable steps toward reducing OCD symptoms rather than dwelling on the problem.
- TF-CBT – Trauma-Focused Cognitive Behavioral Therapy for OCD: Supports individuals whose OCD is linked with trauma by addressing both trauma responses and compulsions.
OCD Treatment for Children
OCD doesn’t just affect adults; it can appear in children too. Many kids experience intrusive thoughts or ritualistic behaviors that cause distress and interfere with school, friendships, or family life. Parents may notice their child repeatedly checking things, avoiding certain places, or needing routines “just right” in order to feel safe.
Signs of OCD in kids may include:
- Excessive handwashing, checking, or counting rituals
- Difficulty completing schoolwork due to intrusive thoughts
- Needing things arranged in a specific order to feel calm
- Intense anxiety or meltdowns when routines are disrupted
At Mountains Therapy, we provide treatment for kids ages 6 and up using developmentally appropriate approaches. Therapy often involves:
- CBT (Cognitive Behavioral Therapy) for OCD: Helping kids recognize obsessions and resist compulsions
- ERP (Exposure and Response Prevention): Supporting children as they face fears gradually without relying on rituals
- Play therapy and creative techniques: Allowing younger children to express worries in a safe, age-appropriate way
- Parent involvement: Teaching caregivers how to support their child without reinforcing OCD behaviors
👉 Early intervention makes a big difference. With support, children can learn to manage OCD symptoms, build resilience, and develop healthier coping strategies that benefit them long-term.
FAQs About OCD
Can OCD be cured?
OCD is highly treatable, though it often requires ongoing management. Many people see significant improvement with therapy.
Is OCD the same as perfectionism?
No. While perfectionism can exist without OCD, OCD involves intrusive thoughts and compulsions that cause distress.
What’s the best treatment for OCD?
Exposure and Response Prevention (ERP), a type of CBT, is considered the gold standard, often combined with other therapies.
Does medication help with OCD?
Yes, medication can be helpful for some individuals with OCD. Doctors may prescribe medications such as SSRIs (Selective Serotonin Reuptake Inhibitors) to reduce obsessive thoughts and compulsive urges. Medication is often used
alongside therapy rather than on its own, as therapy teaches long-term coping skills to break the OCD cycle.
Is medication necessary for OCD?
Not always. Many people benefit from therapy alone, especially approaches like
Exposure and Response Prevention (ERP), which is the gold standard for OCD treatment. However, for some individuals, medication (such as SSRIs) can help reduce symptoms and make therapy more effective. The decision to use medication depends on the severity of symptoms and personal preference.
Final Takeaway
Overall, Obsessive-Compulsive Disorder is not just “habits” that people have. It’s a strong cycle made up of conditioned behaviors and learned responses.
- Professionals use classical and operant conditioning to understand the OCD cycle.
- Therapy helps weaken this cycle and teaches healthier coping mechanisms.
- Even if you’re not a professional, understanding how these cycles work helps explain how fears form and why compulsions are so reinforcing.
👉 As a whole, this helps everyone better understand how exposure therapy works and its importance in treating OCD.
At the end of the day, OCD is treatable—people just need to want treatment.
💡 Remember: You are not alone.
You Are Not Alone!
If you’re unsure whether you want to start therapy or just want to learn more, Mountains Therapy is here for you.
📌 Reach out to connect with a therapist who truly understands what you’re going through.