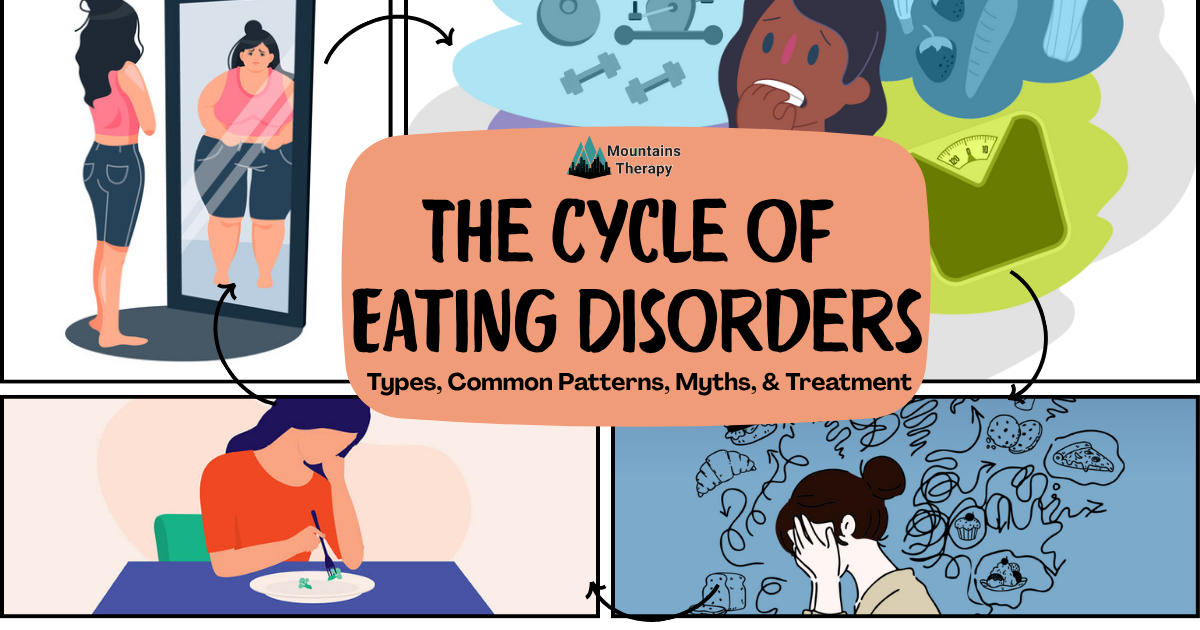
Understanding Eating Disorders: An Analysis of Types, Psychological Factors, Common Patterns, Myths, & Treatment
Learn more about Individual Therapy.
In This Blog, You’ll Learn:
✅ What eating disorders are and how they affect daily life
✅ Psychological factors of eating disorders
✅ Common patterns of eating disorders
✅ Types of eating disorders
✅ Myths vs. facts about eating disorders
✅ How therapy helps with eating disorders
What Are Eating Disorders and Why Does It Matter?
Eating Disorders are more than just overeating- it’s a complex disorder that does involve overeating an uncomfortably large amount of food. But it also captures restrictions of food intake, unhealthy body weight to the point of the development of physical harm or illnesses, on top of the mental health and social impact.
Even though eating disorders are recognized by the DSM as having significant behavioral components, these disorders can increase an individual’s chances of comorbidity with other mental health issues. This includes substance abuse, depression, and anxiety, while also heightening the risk of suicide. From an emotional perspective, these disorders introduce low self-esteem, feelings of loneliness or helplessness, and overall distressing emotions that become difficult to cope with.
What Eating Disorders Are There?
There are four main types of Eating Disorders, excluding childhood eating disorders that are typical for children or adolescents. The Eating Disorders that are listed below have an age of onset of 12 to 25 years of age. But this doesn’t mean someone can’t fall outside of this range.
1. Anorexia Nervosa
Has three sets of criteria that an individual has to meet:
- Restricting/Not getting enough energy intake sufficient for your body, or significant weight loss (according to the DSM-5-TR, significant weight loss is represented by a BMI 17).
- Intense fear of gaining weight or becoming fat, or engaging in behavior that limits weight gain (e.g., overly exercising, fasting).
- Body Image Disturbance: misperception of the body, body shape, overly influences self-evaluation, or lack of recognition of the seriousness of the current low weight.
→ For a diagnosis, Anorexia Nervosa has two types:
- Anorexia Nervosa Restrictive Type;
- In the past 3 months, no recurrent binge eating or purging episodes.
- Weight loss due to behaviors that limit weight gain, like overexercising, fasting, or dieting.
- Anorexia Nervosa Binge Eating/Purging Type;
- In the past 3 months, recurrent episodes of binge eating or purging.
2. Bulimia Nervosa
Five sets of criteria:
- Recurrent binge eating;
- A discrete period of eating an uncomfortably large amount of food
- Perceived lack of control during binge eating
- Engage in Compensatory Behaviors;
- E.g., Vomiting, Usage of laxatives, excessive exercise, Fasting, Enemas, diuretics, etc.
- Criteria A and B must occur at least once per week, for at least 3 months.
- Self-evaluation is unduly influenced by body shape and weight;
- Those with Bulimia usually fall within a normal weight or slightly overweight BMI.
- Does not have Anorexia Nervosa
3. Binge Eating Disorder
- Recurrent Binge Eating
- Binges associated with 3 or more of these:
- Rapid Eating
- Eating till uncomfortably full
- Eating large amounts of food even when not hungry
- Eating alone because of embarrassment about the amount of food
- After a binge, feel disgust, depression, and/or guilt
- Distressed about bingeing
- Frequency: Binge at least 1 time per week on average, for at least 3 months
- No recurrent compensatory behaviors
4. Other Specified Feeding or Eating Disorder (OSFED)
When an individual doesn’t meet the criteria for any eating disorder, but their symptoms are still causing dysfunction and need treatment, clinicians give them this diagnosis. Types:
- Atypical Anorexia = Meet all criteria for Anorexia, but weight is still above the normal range of BMI.
- Bulimia Nervosa subtype or Binge Eating Disorder subtype = meets the criteria for either Bulimia or Binge Eating Disorder, except for frequency criteria.
- Purging Disorder = Individual only engages in purging behavior, but no binge eating.
- Night Eating Syndrome = recurrent night eating, which is not considered part of Binge Eating Disorder.
Psychological Factors of Eating Disorders
There are many questions surrounding the factors that contribute to eating disorders. This leads people to question: Where do eating disorders start?, Are eating disorders genetic?, How do eating disorders affect the brain?, etc.
Sociocultural Factors
- Representation of body shapes has evolved through time with the “ideal body” being put on the front pages of magazines, television, social media, and more.
- With this culture, especially in the US, body shaming has grown, coming from both peers and sometimes even family.
Psychodynamic Factors
- Psychoanalyst Hilde Bruch developed a psychodynamic theory on eating disorders, claiming that it was due to negative relations between daughter and mother that led to disturbances:
- Ego deficiencies are when an individual has low independence due to a lack of control.
- Perceptual disturbances where the individual has trouble perceiving and interpreting their internal cues concerning hunger.
Cognitive Factors
- Negative beliefs about body shape and weight become “core pathology”. For example,
- Judge themselves disproportionately, which drives the other symptoms of eating disorders.
Behavioral Factors
- Genetic Linkage: Relatives of eating disorder patients are 6 times more likely to develop an eating disorder themselves.
- Overlap with brain circuits: E.g., Reward Pathways regulates our drive to eat, and our Habit Formation Circuitry can develop the habit of binge eating behavior.
- Some evidence of hypothalamic dysfunction. Specifically, an imbalance in the lateral hypothalamus produces hunger & the ventromedial hypothalamus reduces hunger sensations.
Biological Factors
- Genetic linkage — relatives of those with eating disorders are 6x more likely to develop one
- Brain circuit overlap — altered reward pathways and habit formation circuits
- Possible dysfunction in hunger regulation via the hypothalamus
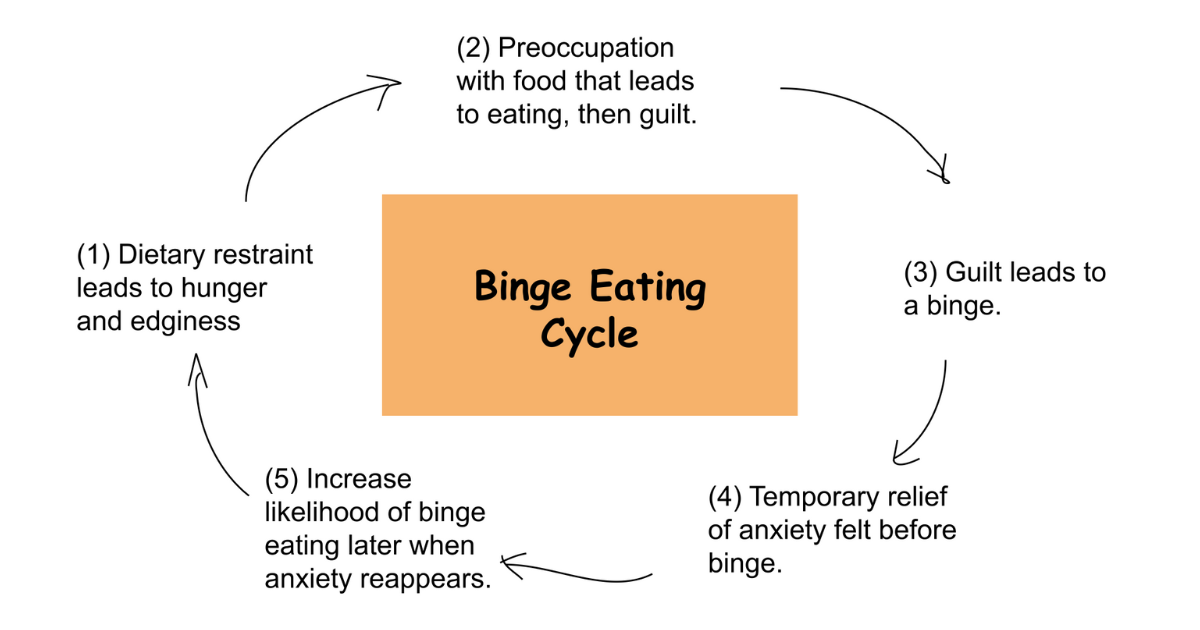
Other Common Patterns of Eating Disorders
- Ego-syntonic nature
- Historically, caucasian women were found to report the highest number of eating disorders.
- Recently, this gap has been closing as more research now includes other groups like African American and Latin women.
- Gender patterns:
- About 27% of men who have eating disorders are due to their job or the sport that they participate in.
- Only 13% of women engage in eating disorders due to their job or sport.
- Even though around 90% of reported eating disorders are in females, there are other factors, specifically for women, outside of their job or sport.
- OSFED is the most commonly diagnosed
eating disorder
Altogether, this is why clinicians must come up with a treatment plan, including therapy and other modalities, to help you identify and reframe these patterns of behavior and thoughts. While also addressing the physical harm caused by eating disorders.
Myths and Facts About Eating Disorders
Myth: Everyone who is obese has an eating disorder.
✅ Truth:
- While some people who are classified as having an eating disorder can be obese, that's not 100% the case each time.
- Those who are obese have a physical health condition, where an individual is above the average weight class for their age and height (BMI).
- Eating disorders are classified as mental health conditions where weight is used as a characteristic when diagnosing, but it’s not the only symptom.
- Eating Disorders are made up of unhealthy eating habits, maladaptive thoughts, and cognitive distortions.
Myth: Everyone who overeats also binges.
✅ Truth:
- Many people occasionally overreact, especially during special events or holidays.
- Binge Eating is a more specific and used to classify behavioral mental health disorders (eating disorders).
- To add on, Binge Eating itself is classified as: eating large quantities of food in a short period of time, even when uncomfortably full, having no control, following feelings of distress.
- As a whole, just because an individual overeats from time to time, it doesn’t mean it qualifies as binge eating, let alone Binge Eating Disorder.
Myth: Finding the weight loss plan will cure Binge Eating Disorder.
- ✅ Truth
- A weight loss program won’t cure Binge Eating Disorder because, as discussed, Binge Eating Disorder is more than just a physical health condition.
- Targeting the weight is one thing, but clinicians also have to help the individual change their maladaptive schemas and cognitive distortions to help with their disorder.
Cognitive Distortions of Eating Disorders
All-or-Nothing Thinking
- Black and white thinking patterns.
- E.g., “I’m either skinny or fat,”
- “I ate a cookie, might as well binge.”
Personalization
- Irrationally blaming yourself for things out of your control, or irrationally blaming others for things that were your fault.
- E.g., “I never heard back after that interview because they judged my body.”
Labeling:
- A negative label to oneself or others.
- E.g., “ I have no self-control when it comes to food, I am just disgusting.”
- “I have no self-control — I’m disgusting.”
Catastrophizing
- Individuals jump to the worst possible outcome with limited to no evidence.
- E.g., “ I ate junk food all week, I know I must’ve gained 30 lbs.”
How Therapy Helps With Eating Disorders
Many individuals ask, “Why Eating Disorders are bad?”. The word bad isn’t the right terminology, but a better phrasing is that Eating disorders can cause long-term mental and physical health problems. This is especially important when not treated immediately and effectively. Some therapeutic practices that would help with Eating Disorders offered by Mountains Therapy are:
- Cognitive Behavioral Therapy (CBT)
- CBT can help individuals recognize their cognitive distortions from eating disorders and challenge them, after helping the individual change to healthier thought patterns.
- Dialectical Behavioral Therapy (DBT)
- DBT helps those mostly with bingeing symptoms and those with Bulimia. With DBT, there is a specific focus on developing skills to manage distress from the disorder, help control emotions, and to be able to improve and maintain healthy relationships.
These therapeutic practices assist with cognitive thought processes; however, it’s essential to recognize that treatment for eating disorders involves additional steps. We don’t specialize in eating disorders, but these practices are merely a part of what can be included in a comprehensive treatment plan for eating disorders.
You are not alone!
If you're someone dealing with an eating disorder and have just realized you have an unhealthy relationship with food that is causing distress in your life, you don’t have to work through it all alone. Whether you have certain symptoms that you feel fall into one of these disorders or you're unsure about what you're struggling with, Mountains Therapy is here to help guide you. Contact us today to connect with a therapist who truly understands what you're going through.